By Dylan Barnaby
•
05 May, 2024
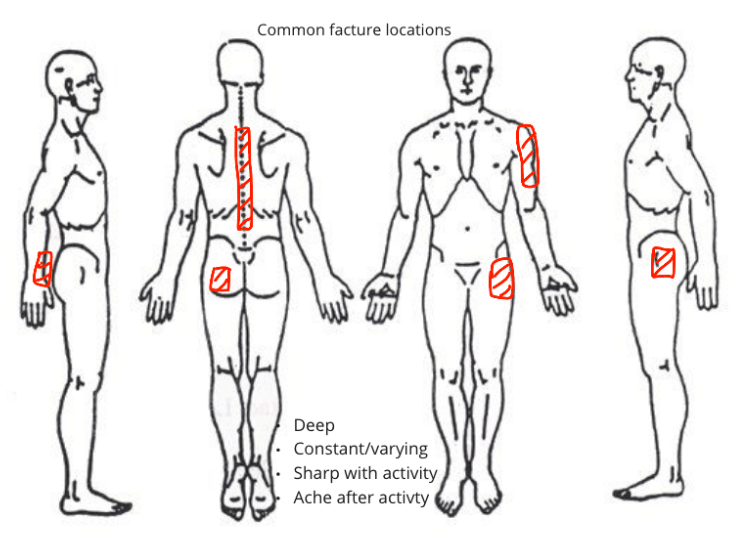
What are the classical features of Osteoporosis? Most common metabolic bone disease in the world. Age: Increased prevalence with age. Thought that due to the aging population societal prevalence is also increasing. Gender: – 16-38% of women over the age of 50 – 3-8% of men over the age of 60 – highest prevalence is post-menopausal women Where is Osteoporosis painful? – Asymptomatic unless a secondary injury has occurred (ie fracture) – Most common sites of osteoporotic fracture include: – Neck of femur – Spine – Radius – Humerus Note: if you observe a cluster of risk factors or the patient is known to have OP then the typical mechanism of injury may not be proportionate to the injury sustained. Therefore need to consider and exclude serious pathology sooner (ie send for imaging) Characteristics of symptoms for Osteoporosis Asymptomatic until a secondary injury – Can be sharp or dull – Can still be asymptomatic with fracture (common in vertebral) – Pain resolves in fracture healing time frames (~6 weeks however can take up to 12 weeks as time frames for osteoporotic fractures are extended) – Pain can radiate from the site of injury (somatic referral) – Can present with neurological symptoms if structures are compromised from secondary injury (ie vertebral fracture) Typical activity capability/restriction for clients with Osteoporosis – If without secondary injury the patient is likely unaffected – Common for patients to have fear of activity if they feel vulnerable (ie they become more sedentary due to a fear of falling, which creates a feedback loop where they are actually at more risk of falling due to deconditioning) – Consider walking aids for high-risk populations to optimise participation and minimise risk – Fractures // can be completely immobilised (ie neck of femur) or asymptomatic (ie vertebral) Neck of femur fracture – Disabling in the elderly population – 25% will need full-time care // nursing home – 20% mortality rate in the 12 months following fracture for those over 60 years old Behaviour of symptoms for Osteoporosis Aggravating: – Specific joint positions // especially towards the end of the range where pressure is increased on the tissues – Loading through an affected joint (ie weight bearing) – If fracture // everything could be painful, multidirectional movement restriction or bias dependant on location – Pain/stiffness after activity Ease – Non-weight bearing positions – Open packed position – Symptoms are often minimal during activity 24-hour pattern: – Morning stiffness <60 minutes – Worse at the end of the day or following activity Typical history of a client with Osteoporosis – Unlikely to report or be aware of the condition in the early stages of progression – Bone density will continue to reduce with age // this is a normal process and hence the age of the patient is a key determinant of the prevalence – Patients with the condition will have increased rates of bone degradation – The rate of degradation will be dependant on individual factors // so attempt to identify those at risk – Risk factors are often characteristics that increase boney degradation – Degradation will determine the fragility of bone – In low-density bones, fractures can occur with minimal stress, hence need to investigate in detail even innocuous events that load boney structures Pathobiological mechanisms behind Osteoporosis Primary contract presentation – Nociceptive dominant – Need to screen for OP and investigate appropriately in the presence of risk factors Risk reduction – Patient asymptomatic – Patient is known to have OP and seeks physiotherapy input to reduce the risk of secondary injury Secondary to injury – Patient has sustained a secondary injury (ie fracture) due to OP – Nociceptive dominant – Need to manage symptoms, optimised healing, reintroduction of load, resume ADL’s and participation, prevention of subsequent injury Proposed pathology underlying Osteoporosis – Mechanism is related to a reduction in bone density. – When boney degradation is greater than boney resorption a person’s density will reduce. – It is normal to go through periods of time where degradation will out way resorption (menopause) however if sustained bone will become osteoporotic. – Two types of OP – Primary OP ( Bone degeneration due to normal bodily processes) can occur in both males and females of all ages. Often occurs in menopausal women and occurs later in life in men. – Secondary OP is a result of medications (eg, glucocorticoids), other conditions (eg, hypogonadism), or diseases (eg, celiac disease). Physical impairments & associated structure/tissue sources (ie P/E findings) Diagnosis will be made by the patient’s doctor. Important to refer for further investigation if the condition is theorised by the physiotherapist. Physiotherapy objective assessment without the presence of a secondary injury will be unremarkable. An analysis is required to identify risk factors to injury or if the patient has already sustained an injury. Imaging – DXA is likely to show reduced bone density, see below for classification Screening – Fracture risk assessment tool FRAX validated and predictive of fracture risk Risk factor assessment performed by physio: – Balance // BERG balance test – Mobility aid // BERG balance test – 6-minute walk test // deconditioning – BMI calculation // online calculator Typical contributing factors to Osteoporosis Non-modifiable – Age – gender – Family history History of previous fracture – Endocrine disorders – Inflammatory disease Modifiable – Low BMI – Smoking – Alcoholism – Nutrition – Medications – Reduced physical activity Relevant precautions/ contraindications to P/E and treatment – Severity and irritability – Serious pathology needs to be excluded – High impact activities (ie jumping or running) – Set up when challenging balance ie (bars) – Neurological symptoms – Falls risk factors – Comorbidities – General conditioning Relevant diagnostic imaging for Osteoporosis Dual-energy x-ray absorptiometry (DXA) is the most common instrument used and is supported by the world health organisation. It determines bone mineral density. – T-score of –1 to –2.5 SD = osteopenia – T-score of less than –2.5 SD = osteoporosis – T-score of less than –2.5 SD with fragility fracture(s) = severe osteoporosis The regular screen is recommended for men over 70 and women over 65 – send to GP for monitoring – If risk factors are present within the patient presentation, send for scans. – If the patient has OP and has a fall recommended to send for further investigation regardless of symptoms Typical prognosis for Osteoporosis – The earlier the condition is identified the more favourable the prognosis – Interventions are able to change metabolic processes involved in the loss of bone density – If not identified until later stages of progression changes in bone density are harder to reverse – Can address modifiable risk factors to reduce the likelihood of subsequent injury regardless of the stage of disease – No cure – Injuries that are associated with high levels of disability have a poor prognosis – Neck of femur fracture after 60 years of age has a 21% mortality rate within 12 months Management/treatment selection for Osteoporosis Nutrition (high-level evidence) – well-balanced diet – maintaining a regular BMI – emphasis on vitamin D and calcium intake Exercise (high-level evidence) – general exercise 5 x 30min weekly – balance // correlation with reduced falls risk – the earlier exercises are commenced // positively correlated to bone density – weight-bearing exercise increased stimulation of bone resorption Pharmacological intervention (high-level evidence) – supplements for vitamin D and calcium – endocrine modulators – common antiresorptive medications that aim to reduced boney degradation include: bisphosphonates, estrogen agonist/ antagonists, estrogens, calcitonin, and denosumab – common anabolic medications that aim to increase bone resorption include teriparatide – Note: Pharmacological treatment is not within the scope of physiotherapy. However, physiotherapists should have an awareness of what medications patients are taking and their side effects. This will enable therapists to flag when the desired outcome may not have been eventuated or adverse effects have occurred. Falls prevention (high-level evidence) – education and reducing risk factors (vision, balance, footwear, environment, dementia) – mobility assessment (ie BERG) – prescription of mobility aids (walking stick, frames, walkers, wheelchairs) Differential diagnosis for Osteoporosis – Cancer // imaging, constant and severe pain, night pain – Infection // history taking and constitutional symptoms – Osteomalacia // vitamin D blood test – Hyperparathyroidism // blood test – Paget’s disease // more specific to one area, BMD investigations – Osteonecrosis // specific to one area, will have evidence of compromised blood supply